There is substantial research available on the ineffectiveness of popularized and politicized non-pharmaceutical interventions. The latest comes from Baruch Vainshelboim, care of the National Institutes for Health (yes, Fauci’s NIH).
Related: Mask Mandates Are Sickening … in the Medical Sense.
The conclusion?
Masks and face coverings serve no public health benefit and come with potential physical and mental health risks. A matter for more than casual consideration because claiming they do have some benefit probably violates federal law.
As for the Vainshelboim Paper, Ed Mosca touched on it here, but I’ll revisit the report’s conclusions and add a bonus. First,
The existing scientific evidences challenge the safety and efficacy of wearing facemask as preventive intervention for COVID-19. The data suggest that both medical and non-medical facemasks are ineffective to block human-to-human transmission of viral and infectious disease such SARS-CoV-2 and COVID-19, supporting against the usage of facemasks.
Wearing facemasks has been demonstrated to have substantial adverse physiological and psychological effects. These include hypoxia, hypercapnia, shortness of breath, increased acidity and toxicity, activation of fear and stress response, rise in stress hormones, immunosuppression, fatigue, headaches, decline in cognitive performance, predisposition for viral and infectious illnesses, chronic stress, anxiety and depression. Long-term consequences of wearing facemask can cause health deterioration, developing and progression of chronic diseases and premature death.
Governments, policy makers and health organizations should utilize prosper and scientific evidence-based approach with respect to wearing facemasks, when the latter is considered as preventive intervention for public health.
To summarize the summary, there is more than enough evidence that making people wear masks does not accomplish any stated political or public health goals. Wearing them has negative mental and physical effects (for no measurable public health gain) a view held the world over.
Again, this is not news. We’ve been sharing similar data for nearly a year while the healthstapo peddles cult-like mask-wearing as a public good.
Or should I say occult? Of, relating to, or dealing with supernatural or magical influences, agencies, or occurrences. … Beyond the realm of human comprehension; inscrutable.
The public health equivalent of astrology with apologies to astrologists for lumping them in with maskholes.
No amount of nagging or nattering or signs or outrage will make them more than what they are which is a physical manifestation of your willingness to participate in a political cult.
Stop.
What, you need more? How about this bonus, as promised? Most of the linked or cited research we’ve published over the year on the inability of masks to achieve any of the wonders attributed to them.
They do not protect you, or anyone around you.
- Ritter et al., in 1975, found that “the wearing of a surgical face mask had no effect upon the overall operating room environmental contamination.”
- Ha’eri and Wiley, in 1980, applied human albumin microspheres to the interior of surgical masks in 20 operations. At the end of each operation, wound washings were examined under the microscope. “Particle contamination of the wound was demonstrated in all experiments.”
- Laslett and Sabin, in 1989, found that caps and masks were not necessary during cardiac catheterization. “No infections were found in any patient, regardless of whether a cap or mask was used,” they wrote. Sjøl and Kelbaek came to the same conclusion in 2002.
- In Tunevall’s 1991 study, a general surgical team wore no masks in half of their surgeries for two years. After 1,537 operations performed with masks, the wound infection rate was 4.7%, while after 1,551 operations performed without masks, the wound infection rate was only 3.5%.
- A review by Skinner and Sutton in 2001 concluded that “The evidence for discontinuing the use of surgical face masks would appear to be stronger than the evidence available to support their continued use.”
- Lahme et al., in 2001, wrote that “surgical face masks worn by patients during regional anesthesia, did not reduce the concentration of airborne bacteria over the operation field in our study. Thus they are dispensable.”
- Figueiredo et al., in 2001, reported that in five years of doing peritoneal dialysis without masks, rates of peritonitis in their unit were no different than rates in hospitals where masks were worn.
- Bahli did a systematic literature review in 2009 and found that “no significant difference in the incidence of postoperative wound infection was observed between masks groups and groups operated with no masks.”
- Surgeons at the Karolinska Institute in Sweden, recognizing the lack of evidence supporting the use of masks, ceased requiring them in 2010 for anesthesiologists and other non-scrubbed personnel in the operating room. “Our decision to no longer require routine surgical masks for personnel not scrubbed for surgery is a departure from common practice. But the evidence to support this practice does not exist,” wrote Dr. Eva Sellden.
- Webster et al., in 2010, reported on obstetric, gynecological, general, orthopedic, breast, and urological surgeries performed on 827 patients. All non-scrubbed staff wore masks in half the surgeries, and none of the non-scrubbed staff wore masks in half the surgeries. Surgical site infections occurred in 11.5% of the Mask group, and in only 9.0% of the No Mask group.
- Lipp and Edwards reviewed the surgical literature in 2014 and found “no statistically significant difference in infection rates between the masked and unmasked group in any of the trials.” Vincent and Edwards updated this review in 2016 and the conclusion was the same.
- Carøe, in a 2014 review based on four studies and 6,006 patients, wrote that “none of the four studies found a difference in the number of post-operative infections whether you used a surgical mask or not.”
- Salassa and Swiontkowski, in 2014, investigated the necessity of scrubs, masks, and head coverings in the operating room and concluded that “there is no evidence that these measures reduce the prevalence of surgical site infection.”
- Da Zhou et al., reviewing the literature in 2015, concluded that “there is a lack of substantial evidence to support claims that facemasks protect either patient or surgeon from infectious contamination.”
And a few more here: (see also here)
- A May 2020 meta-study on pandemic influenza published by the US CDC found that face masks had no effect, neither as personal protective equipment nor as a source control. (Source)
- A Danish randomized controlled trial with 6000 participants, published in the Annals of Internal Medicine in November 2020, found no statistically significant effect of high-quality medical face masks against SARS-CoV-2 infection in a community setting. (Source)
- A July 2020 review by the Oxford Centre for Evidence-Based Medicine found that there is no evidence for the effectiveness of cloth masks against virus infection or transmission. (Source)
- A May 2020 cross-country study by the University of East Anglia (preprint) found that a mask requirement was of no benefit and could even increase the risk of infection. (Source)
- An April 2020 review by two US professors in respiratory and infectious disease from the University of Illinois concluded that face masks have no effect in everyday life, neither as self-protection nor to protect third parties (so-called source control). (Source)
- An article in the New England Journal of Medicine from May 2020 came to the conclusion that cloth face masks offer little to no protection in everyday life. (Source)
- An April 2020 Cochrane review (preprint) found that face masks didn’t reduce influenza-like illness (ILI) cases, neither in the general population nor in health care workers. (Source)
- An April 2020 review by the Norwich School of Medicine (preprint) found that “the evidence is not sufficiently strong to support widespread use of facemasks,” but supports the use of masks by “particularly vulnerable individuals when in transient higher risk situations.” (Source)
- A 2015 study in the British Medical Journal BMJ Open found that cloth masks were penetrated by 97% of particles and may increase infection risk by retaining moisture or repeated use. (Source)
- An August 2020 review by a German professor in virology, epidemiology and hygiene found that there is no evidence for the effectiveness of cloth face masks and that the improper daily use of masks by the public may in fact lead to an increase in infections. (Source)
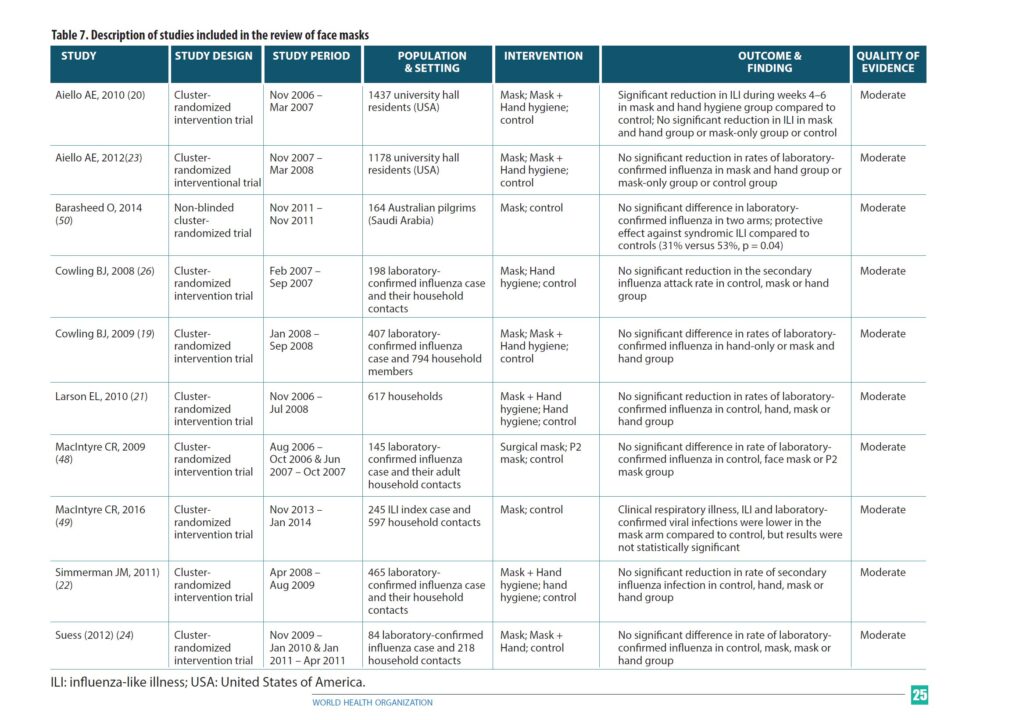
Here’s an image of a matrix referencing more studies (none of which could prove any evidence of a reduction in infections).
More data here care of the CDC that there’s no clinical advantage or benefit to wearing a face covering, and again, here.
None of this will persuade the Covidistas that their crusade is ill-conceived and fraught with dangers. But it might convince a few folks who are either on the fence or have grown weary of the maskholes, the inconvenience or are simply unconvinced that this is the crisis advertised.
It’s not, but even if it were, that does not empower the state to deny you your natural rights. Anyone who believes otherwise needs an electoral exit strategy to get them out of office before they can do more damage.