On Saturday night an elderly resident of a NH long-term care facility fell down and couldn’t get herself back up. It’s actually an independent living facility, but “unfortunately” the Governor’s decrees don’t make that distinction.
Related: New Hampshire COVID19 Threat Index Update 12/15/2020
The ten-month Covid shutdown has been brutal on the elderly. Loss of muscle tone due to sitting alone in solitary confinement for months made it impossible for this elderly resident to get herself off the floor after falling. Just another one of many “unforeseen” costs of the Governor’s State of Emergency.
There was no staff on call after 7 pm, so the Derry police were called at 8 pm and an ambulance arrived to help the resident get up off the floor. That should have been the end of it, but the emergency team decided to bring the resident to the hospital as one ankle appeared swollen, which was difficult to determine given that the resident has considerable edema (swelling due to water retention) in both legs.
After two hours at the hospital, the patient’s designated caretaker, a family member, arrived from out of town to bring the patient back home after being discharged. As we all know, hospitals no longer allow family members inside, unless accompanying a minor. A phone number was provided to the family member at the Emergency Room entrance to call the ER nurse from outside the hospital building.
However, this nurse didn’t want to discharge the patient at 10 pm. An x-ray had been taken, but it had not been reviewed. The family member agreed to bring the patient back to the hospital the next morning in the very unlikely case that there was a fracture. It was very late in the evening and the patient was exhausted.
The nurse argued that bringing the patient back to the hospital a second time would result in twice the exposure to Covid. The family member argued that staying twice as long in the hospital for what was very likely only a minor sprain was also unnecessary exposure to Covid.
The nurse didn’t allow the family member to speak to the patient by phone despite several requests to do so. As the patient wasn’t aware that a family member was at the hospital to pick her up, the nurse had complete control over the situation. The family member’s concerns could be safely ignored.
The nurse stated that the patient wanted to say in the hospital waiting for the results and to have a meal, even though the nurse was informed that a meal was waiting for the patient in her apartment back home.
Next, the police tell the family member, who was standing outside in the dark, nearly empty, parking lot, that she must return to her car — otherwise, they would be forced to call the police station and have her arrested.
There was no one outside to endanger. What law had been broken, the family member asked?
After some hemming and hawing, because the Governor’s decrees are in fact not law and the police know it, they finally threatened that she would be arrested for “disorderly conduct.”
Asking questions at a hospital and trying to be a good caretaker for an elderly relative is now considered “disorderly conduct.” This is what happens when the police are told to vigorously enforce the Governor’s emergency diktats.
A responsible caretaker might worry about what medications were given to the patient at the hospital without the patient’s or caretaker’s knowledge.
This particular caretaker has first-hand experience with opioids being given to patients without any disclosure during a previous hospital visit. What type of extraneous tests were administered? The elderly are frequently targets of over-testing due to their trusting nature and ample medical coverage. It’s long past the time when you could trust hospitals to make patient welfare their priority. Now it’s often the bottom line and keeping patients docile.
Finally, at 11 pm, the patient was discharged with paperwork indicating that it was just a sprain. It was also apparent that the patient had no knowledge that a family member had been waiting outside the hospital for an hour.
The discharge nurse did not push the patient out of the hospital in a wheel chair, which is standard practice, whether the patient is capable of walking or not. This 95-year-old tired and disoriented patient walked out of the hospital on her own, slowly pushing her walker.
The patient then slept 15 hours straight and had no appetite for two days. What was she given at the hospital that would knock her out and undermine her appetite? An opioid for a sprained ankle?
It’s far past time to end the State of Emergency in New Hampshire. The Constitution has been suspended. We are living in a police state where the rule of law no longer exists.
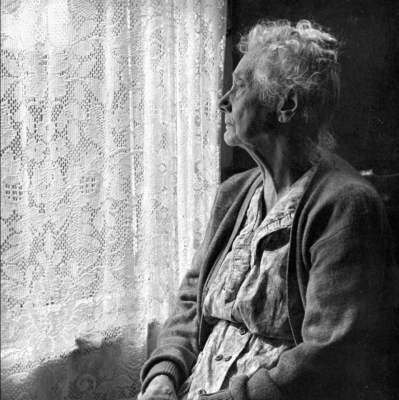
Photo by Chalmers Butterfield